CASE 4: A 70yr old male with swelling over right lower limb
Hi, I am P. Shreya Reddy, 5th semester medical student.
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CONSENT AND DE-IDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed throughout the piece of work whatsoever.
A 70yr old male came to the OPD
with C/o swelling over right lower limb.
- c/o pain and swelling over Right LL, shortness of breath (Grade 2) since 2 days
- No aggravating and relieving factors.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 2 days ago and then developed blebs and swelling in Right Lower limb
-H/o trauma present and was subsided on medication
-Pain was of sudden onset and gradually progressive with no aggravating and relieving factors
- K/c/o DM Type-2 since 2 years and is on regular specific medication (metformin hydrochloride and glimepiridine tablets- GLIMP M2)
- K/C/o HTN since 1 year and on regular unspecified treatment.
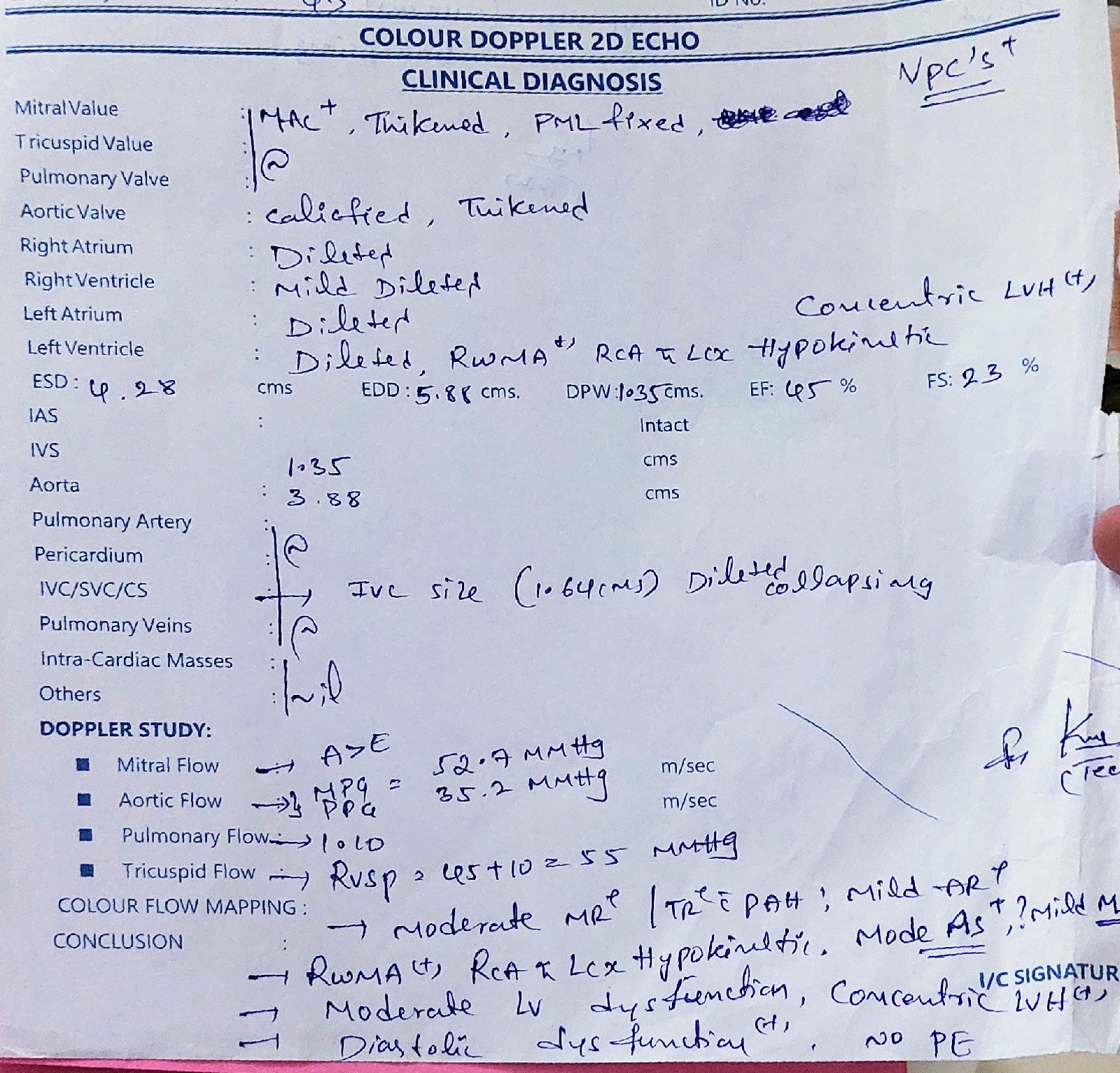
-On 2nd of this month the patient complaint of sudden SoB and was taken to for ECG
- after I/V/O SoB and ECG it's been diagnosed as Cardiomyopathy.
HISTORY OF PAST ILLNESS:
K/c/o DM and HTN
Not a k/c/o epilepsy, asthma, TB and Thyroid.
SURGICAL HISTORY:
- Right inguinal hernia 15 years ago
PERSONAL HISTORY:
- Married
- Appetite normal
- Mixed diet
- Sleep normal
- Bowel and bladder normal
- Addictions: consumed Alcohol specifically beer but stoped 10yr ago.
FAMILY HISTORY
No known cases of:
- diabetes mellitus
- hypertension
- heart disease
- stroke
- cancer
- tuberculosis
- asthma
- other hereditary diseases
GENERAL EXAMINATION:
The patient was examined in well lit room after taking his consent.
- conscious, coherent and co operative.
- well Oriented to time, place and person
- No pallor
- no interus
- no cyanosis
- no clubbing
- no lymphadenopathy
- no edema.
VITALS:
- Temperature: afebrile
- Blood Pressure: 110/70 with inotropic
- Pulse Rate: 106 bpm
- SpO2: 97%
SYSTEMIC EXAMINATION:
Cardiovascular System
- no thrills
- cardiac sounds S1 and S2 heard
- no cardiac murmurs
Respiratory System
- no dyspnea
- no wheeze
- trachea position: central
- breath sounds: vesicular
Abdomen
- soft and tender
- no scars, striae, engorged
- bowel sounds heard
- no bruits, rubs
- no shifting of dullness
- no fluid thrill
- no palpable mass
- hernia orifices: normal
- liver: not palpable
- spleen : not palpable
GIT:
-Bowel sounds: positive
Central Nervous System
- conscious
- coherent
- speech normal
-no meningeal signs
- sensory, motor systems: normal
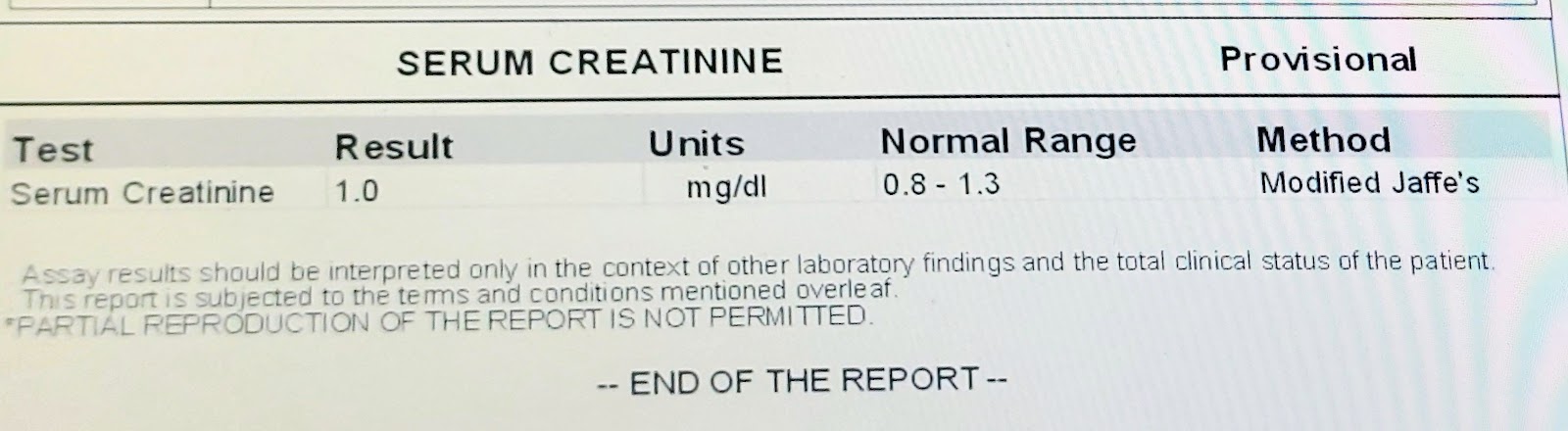
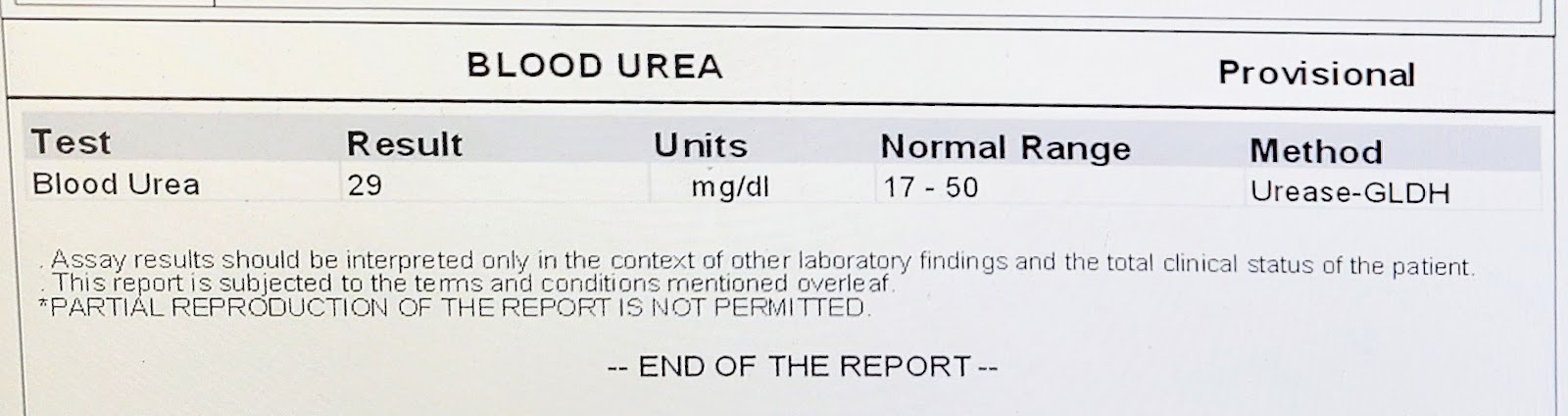
INVESTIGATIONS:
DOPPLER:
ECG:
FEVER CHART:
MEDICATION:
INJ Piptaz- 4.45gm IV/ TID
INJ Clindamycin- 600mg IV/ TIM
INJ Noradrenaline 8ml +42 ml NS (9ml/ hr)
INJ Dobutamine 5ml + 45ml NS (6ml/hr)
INJ Lasix Infusion (5mg/hr)
INJ Thiamine 20mg in 100ml NS IV/BD
Tab Met XL 12.5mg PO OD
PROVISIONAL DIAGNOSIS: Right lower limb cellulitis.