CASE 8: A 68yr old male with right lower limb swelling.
Hi, I am P. Shreya Reddy, 5th semester medical student.
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CONSENT AND DE-IDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed throughout the piece of work whatsoever.
CASE SCENARIO:
A 65yr old male resident of ramanapet , painter by occupation, came to the OPD with the cheif complaints of
- swelling over the right lower limb since 1 week
HISTORY OF PRESENT ILLNESS:
- The patient was apparently asymptomatic 1 week ago, then developed swelling over the right lower limb due to trauma by a thron prick which led to blistering of the trauma site.
- 6 days ago he visited a local doctor who recommended him to go to Kamineni hospital. Upon arriving 5 days ago surgical debriment of the dorsal side of foot was done due to its spread.
- 5 days ago even after surgical removal of debris, the infection started to spread to the surrounding area and now its spread is also seen above the knee level.
- 4 days ago the following conditions presented secondary to swelling and infection:
(i) sepsis
(ii) moderate pleural effusion
(iii) multiple organ dysfunction syndrome [MODS]
(iv) Disseminated intravascular coagulation [DIC]
- history of fever 6days ago
- history of Trauma 1week ago
--> no history of diarrhea, constipation, malena, cough, SOB, burning micturition, reduced urine output.
DAILY ROUTINE:
- Before 1 week, he used to wake up at 4:30am to tend to his cattle, then eats rice for breakfast and goes to work in the fieldas a farmer. At 1pm he used to have lunch (rice). He used to complete his work and come back to his house at around 6:30 - 7pm. He usually had dinner (rice) at 8pm and then went to sleep.
- since 1 week, he wakes up at random times between 5 am to 9 am, is not taking any meals when given by attender and lies in bed most of the time.
HISTORY OF PAST ILLNESS:
- No History of similar complaints present in the past.
- N/K/C/O HTN, DM, TB, CVD, Asthma, Epilepsy, Thyroid disorders, blood transfusions.
SURGICAL HISTORY:
- no pervious surgical history.
PERSONAL HISTORY:
- Married
- farmer by occupation
- Mixed diet
- Appetite decreased since 6 days
- Adequate sleep
- decreased bowel movement
- Normal micturition
- No known allergies
FAMILY HISTORY:
No significant family history
GENERAL EXAMINATION:
I have examined the patient after taking prior consent and informing the patient in the presence of a female attendant. The examination was done in both supine and sitting position in a well lit room.
- patient was conscious, coherent and cooperative
- well oriented to time and space
- poor built and inadequately nourished
- no pallor
- no icterus
- no cyanosis
- no clubbing of fingers
- no lymphadenopathy
- no pedal edema
- no malnutrition
- dehydration moderately present
VITALS:
- Temperature: afebrile
- Pulse rate: 76 bpm, regular rhythm, normal volume
- Respiratory rate: 24 cpm
- BP: 100/60 mm Hg
- SPO2: 98% at RA
SYSTEMIC EXAMINATION:
Cardiovascular System
- no thrills
- cardiac sounds S1 and S2 heard
- no cardiac murmurs
Respiratory System
- no dyspnea
- wheeze present
- trachea position: central
- breath sounds: vesicular
Abdomen
- tenderness present (in the epigastric region)
- shape: scaphoid
- no scars, striae, engorged veins
- bowel sounds heard
- no bruits, rubs
- no shifting of dullness
- no fluid thrill
- no palpable mass
- hernia orifices: normal
- liver: not palpable
- spleen : not palpable
- genitals: normal
Central Nervous System
- conscious
- normal speech
- cranial nerves normal
- motor functions are elicited
- sensory systems normal
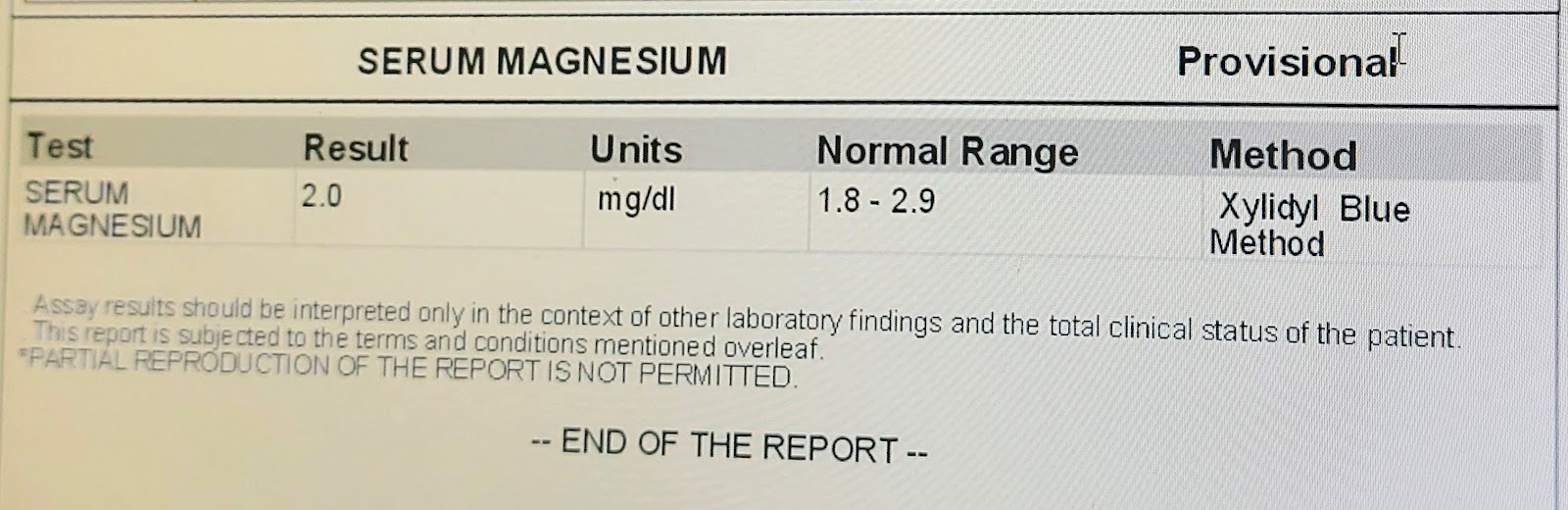
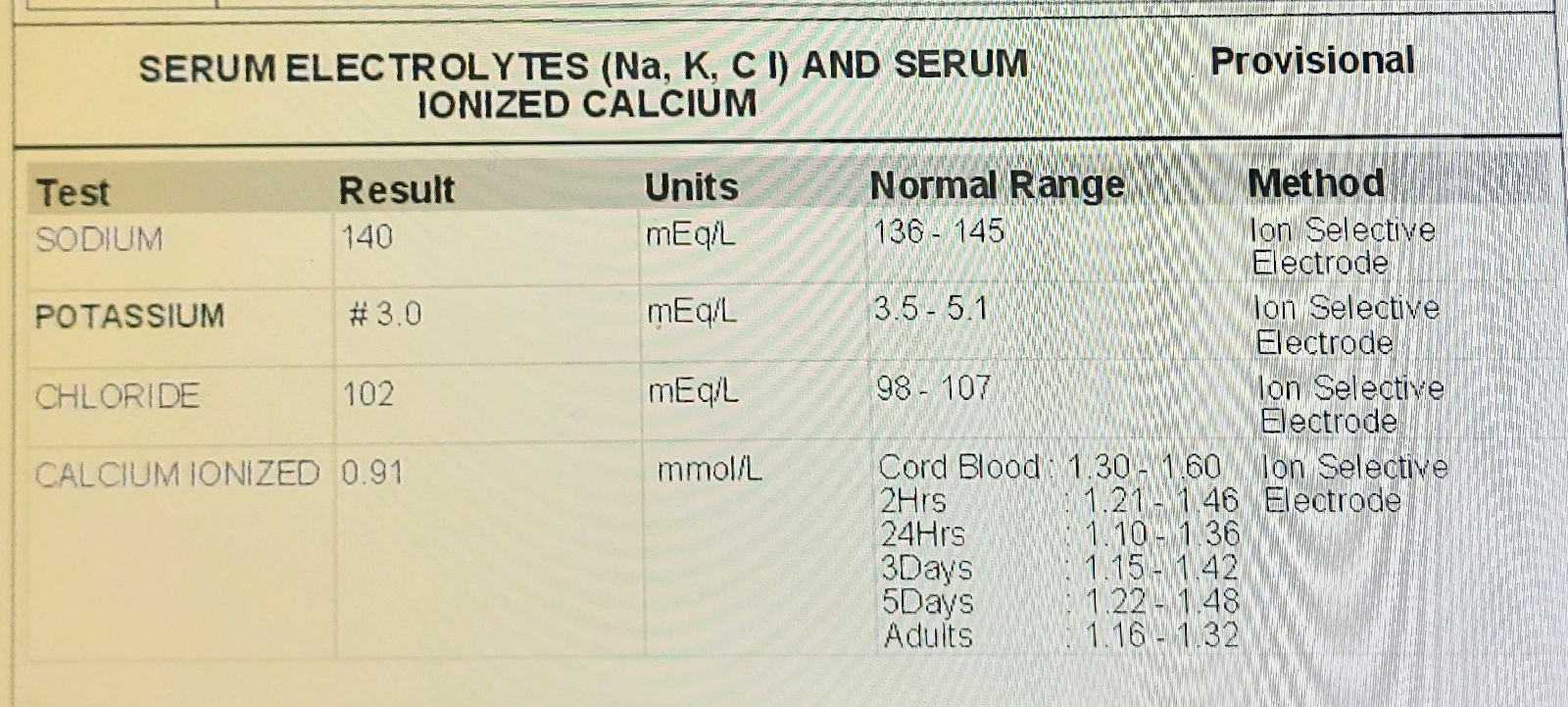
INVESTIGATIONS:
X-ray: on 16th sept, 2023
X-ray: on 18th sept, 2023
PROVISIONAL DIAGNOSIS:
CELLULITIS (surgical debriment), ACUTE KIDNEY INJURY and SEPSIS
TREATMENT:
IV FLUIDS
INJ. OPTIENEURON - 1amp, I.V, once a day
INJ. PEPTAZ - 2.25mg, I.V, thrice a day
INJ. METROGYL - 500mg, I.V, thrice a day
INJ. PANTOP - 40mg, I.V, once a day
SYP. POTKLOR - 10ml, Oral, twice a day
INJ. ZOFER - 4 mg, I.V, thrice a day
TAB.PARACETAMOL- 650mg, Oral, thrice a day
TAB. CHYMOROL FORTE - Oral, thrice a day
NEB. IPRAVENT.
NEB. BUDECORT.