CASE 9: A 65yr old female with urinary incontinence and Rheumatoid arthritis
This is an updated blog done by taking reference from:
https://anahitabehara.blogspot.com/2023/09/63f-urinary-incontinence-4-years-ra-on.html
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CONSENT AND DE-IDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed throughout the piece of work whatsoever.
CASE SCENARIO:
A 65 year old female, resident of west bengal and belonging to middle class according to modified kuppuswamy scale presented to the general medicine OPD with chief complaints of:
-continuous dribbling of urine since the past 4 years
- constipation since past 3 years.
- shortness of breath since 3 years.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 26 years ago , when she developed:
* continuous dull aching pain in both the knee joints, which was exaggerated in the mornings and was bearable throughout the day, it was aggravated on walking and relieved on rest, associated with redness around the knees
- N/H/O trauma
- N/H/O fever with evening rise of temperature, cosmetic deformity(varicosity, skin discoloration)
- later as the disease progressed she underwent bilateral knee replacement surgery in the year 2015.
* continuous dribbling of urine since 4 years, which was insidious in onset with a few drops during the day and gradually progressed to continue throughout the day and wetting of bed during the night, urine is yellow in color with ammonical odour. Aggravated on consumption of coffee & drinking more than 1.5 lit of water.
* patient reports recurrent UTIs where in she complains of
-burning micturition
-pain before and while micturition
-no history of hematuria, frothy urine
* patient also reports constipation since 3 years,
- she passes 1 bowel movement per 2-3 days , associated with pain
- patient passes flatus
- not associated with blood, abdominal distention, weight loss
* fever since 1 day, sudden onset, high grade, continuous, no aggravating and relieving factors, associated with bodyache, headache.
HISTORY OF PAST ILLNESS:
- H/O rheumatoid arthritis since past 26yrs, is on regular medication.
- H/O HTN since past 20yrs on regular medication.
- H/O SOB since past 3years due to seasonal changes (usually in cold weather) and in stressful situations, she uses specified medication (inh. budetrol 400, oxymethazoline hydrochloride nasal drops)
- N/K/C/O DM, TB, CVD, Asthma, Epilepsy, Thyroid disorders, blood transfusions.
SURGICAL HISTORY:
- history of bilateral knee replacement 8 years ago.
- history of LSCS 27yrs ago
PERSONAL HISTORY:
- Married
- Mixed diet
- Decreased appetite due to fullness of abdomen
- Adequate sleep
- Decreased bowel movement lead to constipation since past 3 yrs
- micturition: urinary incontinence since past 4yrs
- No known allergies
- no known addictions
DRUG HISTORY:
- Tab. METHOTREXATE 10mg.
- Tab. FOLIC ACID 5mg.
- Tab. CLINIDIPINE, TELMISARTAN & CHLORTHIDONE.
- Tab. BISOPROLOL FUMARATE.
- Tab. NORTRIPTYLINE, MECOBALAMIN & PREGABALIN.
- Tab. MIRABEGRON Extended release.
- Tab. RAVEPRAZOLE SODIUM 20mg & DOMPERIDONE 30mg.
- Syp. LIQUID PARAFFIN, MILK OF MAGNESIUM & SODIUM PICOSULFATE.
- Inh. BUDESONIDE.
FAMILY HISTORY:
- the patient’s mother and younger sibling are known cases of osteoarthritis
GENERAL EXAMINATION:
I have examined the patient after taking prior consent and informing the patient in the presence of a female attendant. The examination was done in both supine and sitting position in a well lit room.
- patient was conscious, coherent and cooperative
- well oriented to time and space
- well built and adequately nourished
- no pallor
- no icterus
- no cyanosis
- no clubbing of fingers
- no lymphadenopathy
- no pedal edema
- no malnutrition
SYSTEMIC EXAMINATION:
Cardiovascular System
- no thrills
- cardiac sounds S1 and S2 heard
- no cardiac murmurs
Respiratory System
- no dyspnea
- no wheeze
- trachea position: central
- breath sounds: vesicular
- no adventitious sounds heard
Abdomen
- no tenderness
- bowel sounds heard
- no bruits, rubs
- no shifting of dullness
- no fluid thrill
- no palpable mass
- hernia orifices: normal
- liver: not palpable
- spleen : not palpable
Central Nervous System
- conscious
- normal speech
- cranial nerves normal
- motor and sensory systems normal
INVESTIGATIONS:
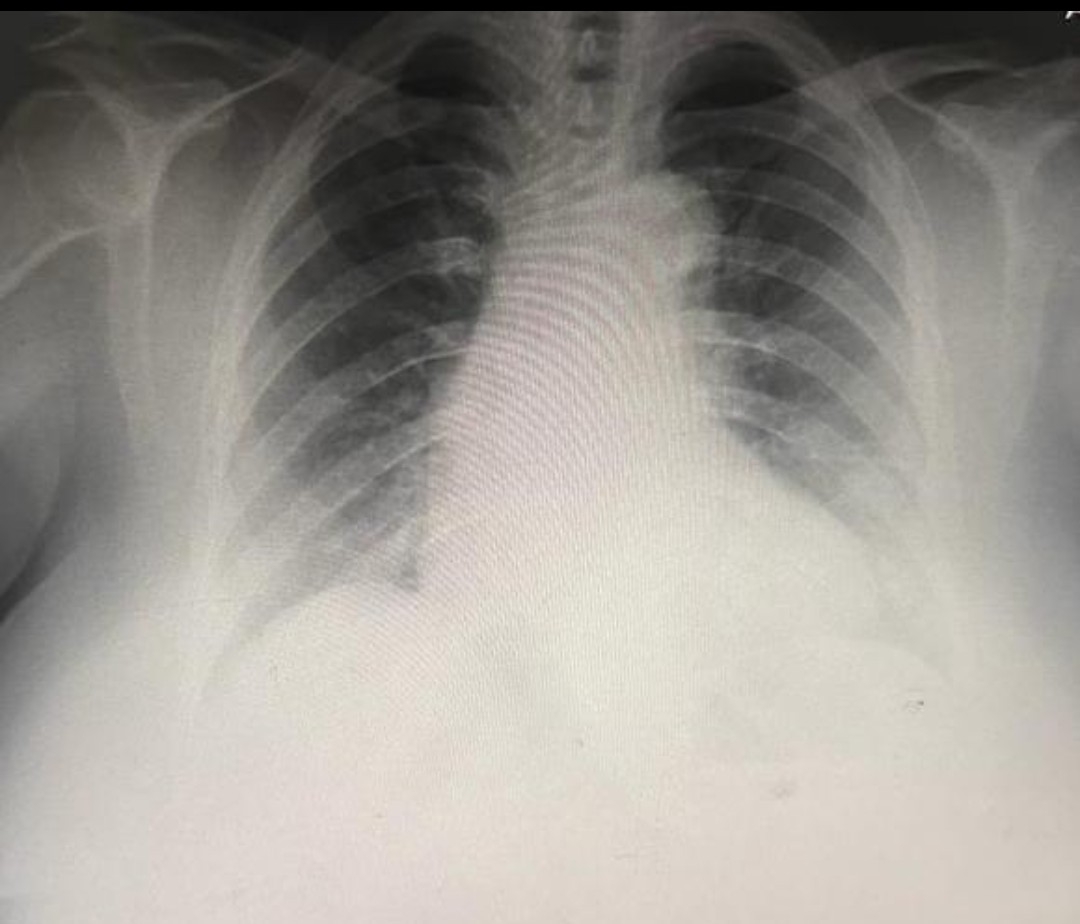
CHEST X-RAY
BILATERAL HAND X-RAY