CASE 6: A 52Y female with Headache, Pain over DIP, elbow, shoulder joints since 1 month
Hi, I am P. Shreya Reddy, 5th semester medical student.
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CONSENT AND DE-IDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed throughout the piece of work whatsoever.
CASE SCENARIO:
A 52 year old female resident of Gasaram village, came to the OPD with chief complaints of:
- Headache since 1 month.
- Pain over the DIP joint, elbow joint and shoulder joint since 1 month.
HISTORY OF PRESENT ILLNESS:
- Patient was apparently asymptomatic 5 years back, then gradually developed pain for the 1st time over the shoulder joint and elbow joint.
* Then 1 month ago she developed:
- headache associated with Neckpain, radiating to B/L upper limbs, which was aggrevated with bending forward and relieved on rest & using unspecified medication.
- Pain over the DIP joint, elbow joint and shoulder joint, B/L symmetrical in distibution, associated with morning stiffness lasting for around 10 to 15 mins.
•N/C/o SOB, chest pain, orthopnea, PND
•N/c/o Fever, diarrhea, constipation, melena, decreased urinary output, burning micturition.
DAILY ROUTINE:
HISTORY OF PAST ILLNESS:
- HTN, DM2, thyroid disorders, Bronchial Asthma, CVA, CAD,TB.
- No history of allergies to food/drugs.
- No history of blood transfusions.
SURGICAL HISTORY:
- no pervious surgical history.
PERSONAL HISTORY:
- Married
- Mixed diet
- Appetite decreased since 1 day
- inadequate sleep
- Regular bowels
- Normal micturition
- No known allergies
- Occasionally (during summer season) consumes toddy (1 or 2 glasses) since 18yrs ago .
FAMILY HISTORY:
No significant family history
GENERAL EXAMINATION:
I have examined the patient after taking prior consent and informing the patient in the presence of a female attendant. The examination was done in both supine and sitting position in a well lit room.
- patient was conscious, coherent and cooperative
- well oriented to time, place and people
- well built and adequately nourished
- no pallor
- no icterus
- no cyanosis
- no clubbing of fingers
- no lymphadenopathy
- no pedal edema
- no malnutrition
- no dehydration
VITALS:
- Temperature: 98.8 F
- Pulse rate: 81bpm
- BP: 120/70 mmHg
- Respiratory rate: 16cpm
On examination of bilateral hands:
- B/L symmetrical DIP Joints
- Pain present
- No tenderness
- No Synovial thickening
- No external deformity
SYSTEMIC EXAMINATION:
Cardiovascular System
- no thrills
- cardiac sounds S1 and S2 heard
- no cardiac murmurs
Respiratory System
- no dyspnea
- no wheeze
- trachea position: central
- breath sounds: vesicular
- no adventitious sounds heard
Abdomen
- tenderness present (in the epigastric region)
- shape: scaphoid
- no scars, striae, engorged veins
- bowel sounds heard
- no bruits, rubs
- no shifting of dullness
- no fluid thrill
- no palpable mass
- hernia orifices: normal
- liver: not palpable
- spleen : not palpable
Central Nervous System
- conscious
- normal speech
- cranial nerves normal
- motor and sensory systems normal
INVESTIGATIONS:
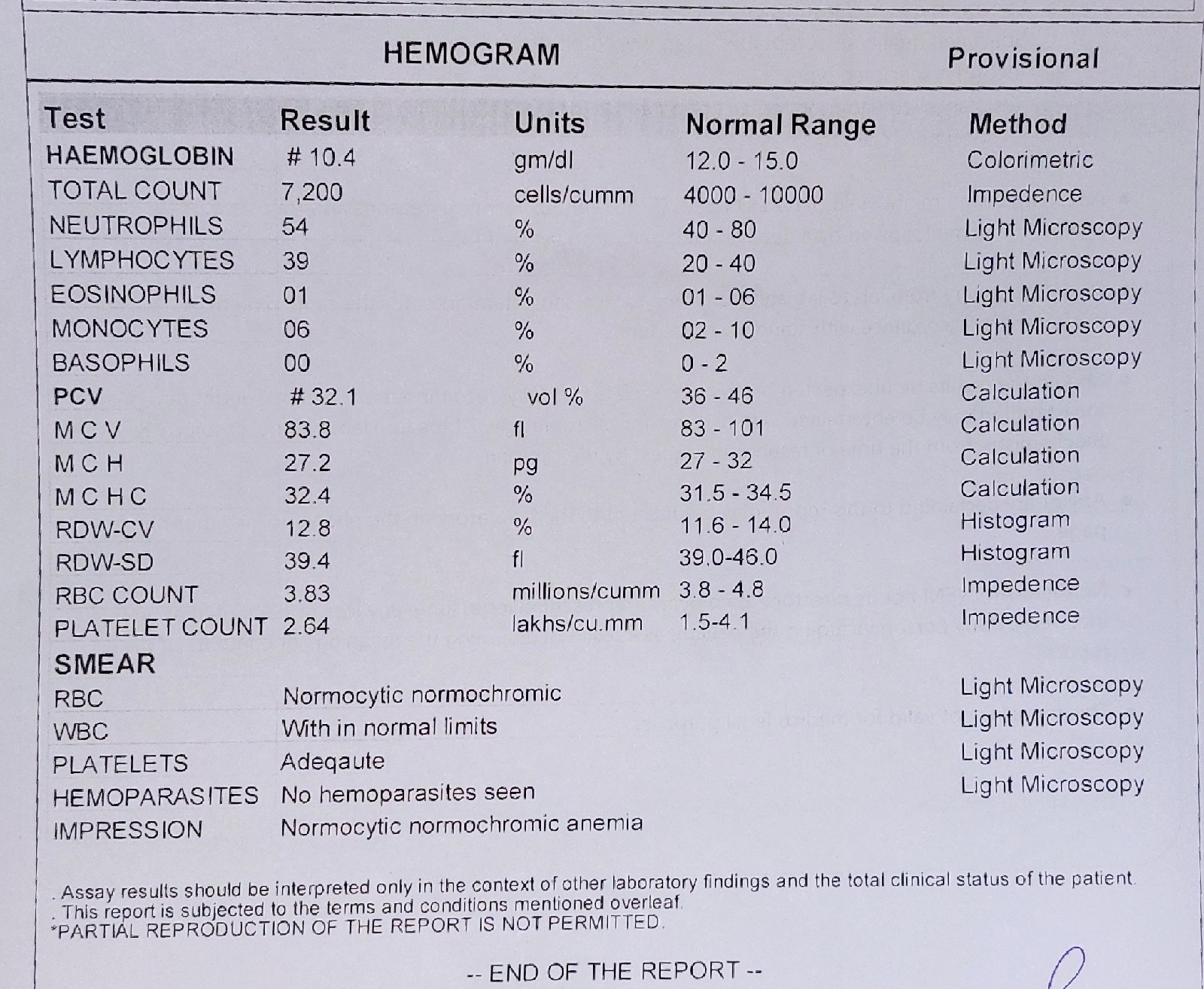
HEMOGRAM:
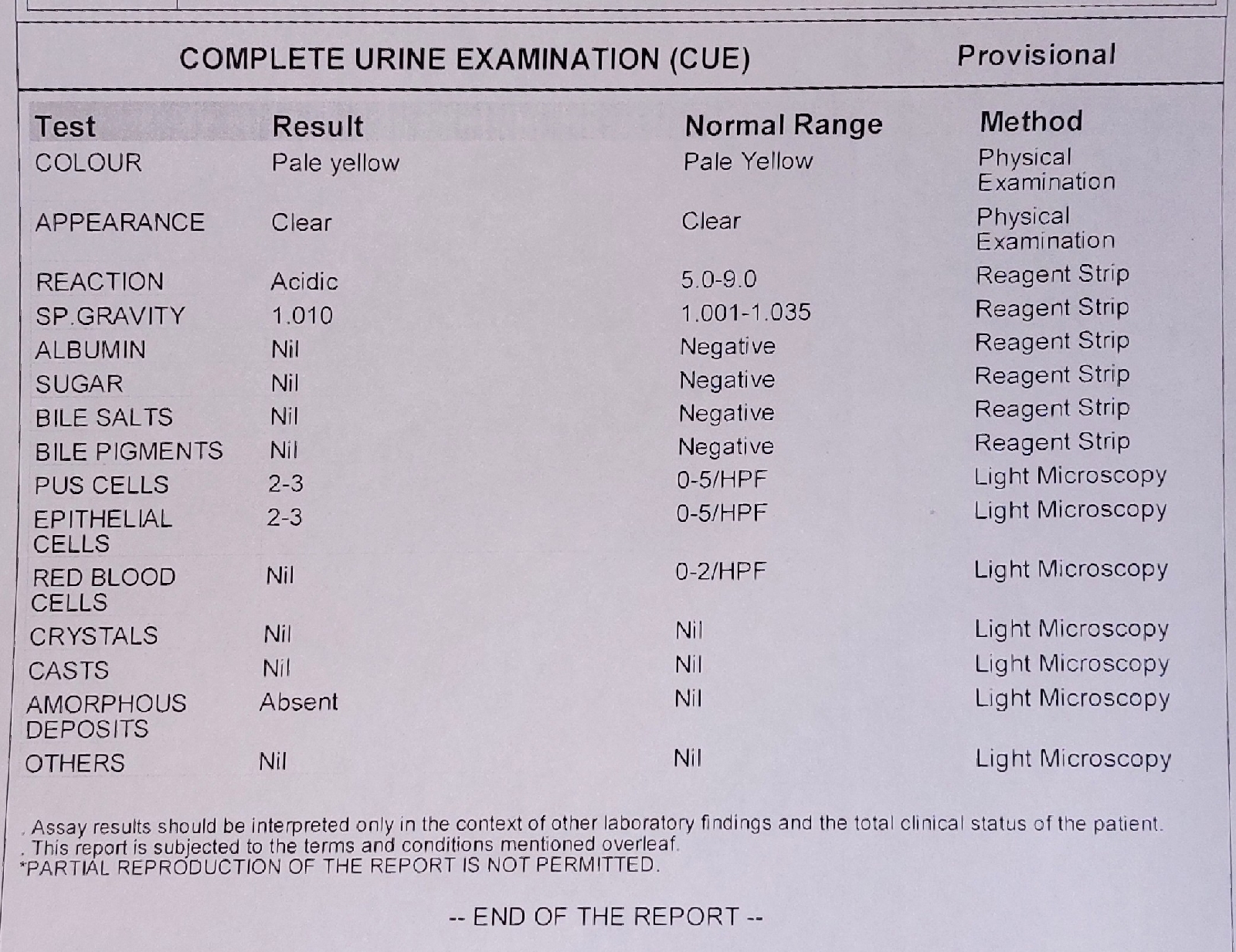
COMPLETE URINE EXAMINATION:
SERUM ELECTROLYTES:
SERUM CREATININE:
BLOOD UREA:
RANDOM BLOOD SUGAR:
TREATMENT:
- Tab. HIFENAC (For pain, NSAID+ Muscle relaxant)
- Tab. MVT (multivitamin)
DIFFERENTIAL DIAGNOSIS:
- Rheumatoid arthritis?
- Cervical spondylitis?
PROVISIONAL DIAGNOSIS: