CASE 7: 60 yr old female with headache since 1 month, fever and productive cough since 10 days
Hi, I am P. Shreya Reddy, 5th semester medical student.
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CONSENT AND DE-IDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed throughout the piece of work whatsoever.
A 60 Year old female, resident of Suryapet, daily wage laborer by occupation came to OPD with chief complaints of
- headache since 1 month
- fever since 10 days
- cough since 10 days.
HISTORY OF PRESENT ILLNESS:
- Patient was apparently asymptomatic 1 year ago when she developed shortness of breath of grade 1, no orthopnea, no PND, no chest pain.
- She had headache since 1 month, of diffuse type in the parietal region which radiates to neck and lower back, associated with productive cough since 10 days, aggravated by exposure to cold weather, not relieved by medication, no diurnal variation, and the sputum is white in colour and mucoid in nature.
- She also has fever since 10 days of high grade, associated with chills and rigor, no sweating, intermittent, no diurnal variations.
- No h/o chest pain, sweating, palpitations, loose stools, nausea, vomiting, burning micturition, decreased urine output and weight loss.
DAILY ROUTINE:
Before she got sick, she used to wake up between 5-6am every morning, cook food, takes a bath, wash clothes and dishes by 8am, eat breakfast of rice and curry and leaves for work by 8.30am. She is a daily wage laborer by occupation and she used to pack lunch (same rice and curry as breakfast) and eat it at her workplace. She used to reach home by 7 or 8pm after which she would cook dinner (rice) , eat and sleep by 11pm.
After she got sick, she stopped going to work and stayed at home, following which she was admitted into the hospital.
HISTORY OF PAST ILLNESS:
- similar complaints 2 months ago of fever, headache and body pain which was relieved on use of unspecified medication.
- N/k/c/o DM, HTN, CAD, TB, epilepsy, asthma, bronchitis.
SURGICAL HISTORY:
- tubectomy was done 20 years ago, later followed by hysterectomy.
PERSONAL HISTORY:
- married
- Mixed diet
- decreased appetite
- regular bowels
- normal micturition
- no known allergies
- addictions: Used to consume toddy but stoped 20 years ago.
FAMILY HISTORY:
- Not significant
GENERAL EXAMINATION:
I have examined the patient after taken prior consent and informing the patient in the presence of a female attendant. The examination was done in both supine and sitting position in a well lit room.
- patient was conscious, coherent and cooperative
- well oriented to time, place and person
- well built and adequately nourished
- pallor present
- no icterus
- no cyanosis
- clubbing of fingers present
- no lymphadenopathy
- no edema of feet
- no malnutrition
- no dehydration
VITALS:
- Temperature: 95°F
- Pulse: 84/min
- RR: 18 cycles/min
- BP: 130/70 mm Hg
SYSTEMIC EXAMINATION:
Respiratory System:
- upper respiratory tract : oral cavity, nose & oropharynx appear normal
- chest is bilaterally symmetrical
- respiratory movements appear equal on both sides and of thoracoabdominal type
- trachea position: central
- breath sounds: vesicular
- wheeze: present in bilateral suprascapular, infrascapular and mammary areas
Cardiovascular System:
Inspection :
- shape of chest : elliptical
- no engorged veins, scars, visible pulsations
Palpation :
-Apex beat can be palpable in 5th intercostal space
- no cardiac thrills
Auscultation :
- S1,S2 are heard
- no murmurs
Abdomen:
- shape: scaphoid
- no tenderness
- no palpable mass
- no bruits
- no free fluid
- hernias orifices: normal
- liver: not palpable
- spleen : not palpable
- no bowel sounds
Central Nervous System:
- conscious
- normal speech
- no meningeal signs
- cranial nerves: normal
- sensory : normal
- motor: normal
- reflexes: all present bilaterally
- gait: normal
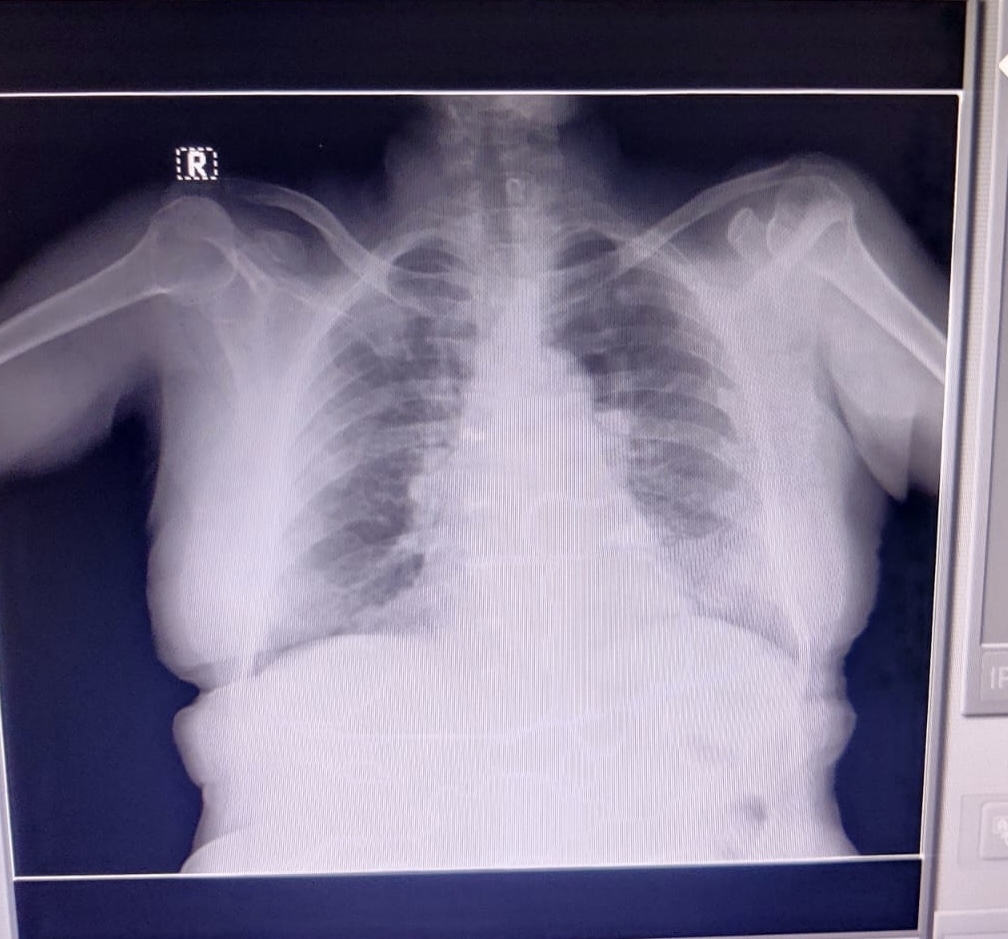
INVESTIGATIONS:
HEMOGRAM:
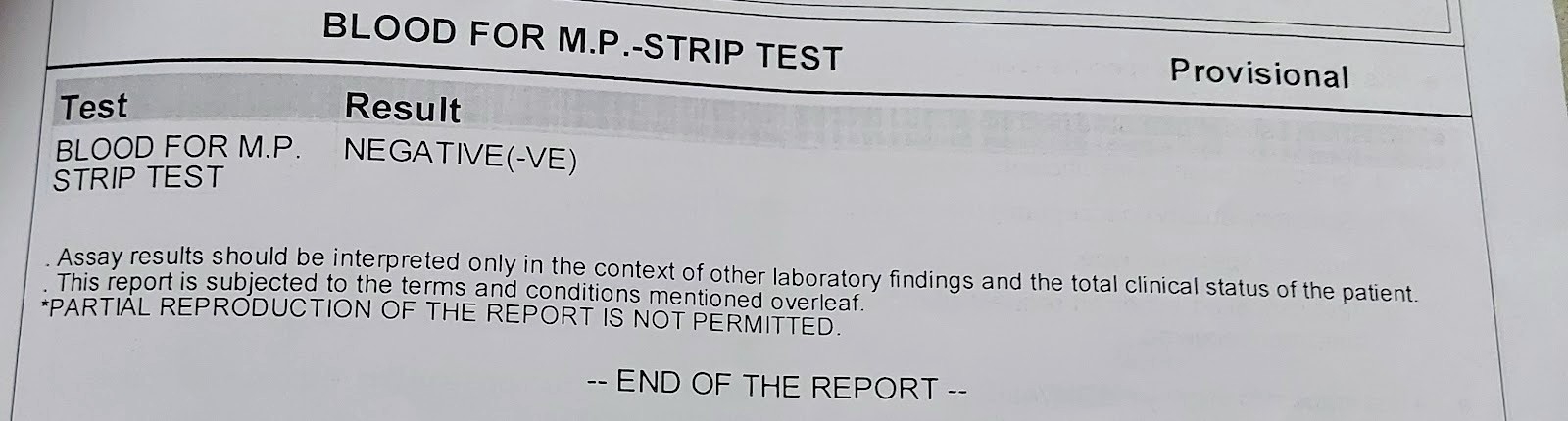
MALARIA PARASITE TEST:
PROVISIONAL DIAGNOSIS:
Pyrexia secondary to lower respiratory tract infection with h/o bronchial asthma (exacerbation)
TREATMENT:
- INJ. Neomal 1gm iv
- TAB. Paracetamol 650mg
- TAB. Levocetrizine
- SYRUP. Ascoril- LS
- TAB. Azithromycin
- TAB. Amoxicillin